Mood
 ATYPICAL DEPRESSION
ATYPICAL DEPRESSION
Actually, all too typical for words.
by John McManamy
Actually, all too typical for words.
by John McManamy
DON'T BE FOOLED. Atypical depression is actually the most common subtype of depression in outpatients, affecting anywhere from 25 to 42 percent of the depressed population.
Atypical Depression Symptoms
Atypical depression debuted in the DSM-IV in 1994, following decades of debate. According to the DSM, as opposed to major depression, the patient with atypical features experiences mood reactivity, with improved mood when something good happens. This would broadly translate to an individual momentarily taking leave of his or her Stygian gloom to laugh at a friend slipping on a banana peel.Likewise, there would be an element of enthusiasm to news of winning the Powerball lottery.
In addition, the DSM-IV mandates at least two of the following: Increase in appetite or weight gain (as opposed to the reduced appetite or weight loss of "typical" depression); excessive sleeping (as opposed to insomnia); leaden paralysis; and sensitivity to rejection.
Sensitivity to rejection could be interpreted as the flip side to mood reactivity. Here, there is a visible response to bad news rather than good. Either way - mood reactivity or sensitivity to rejection - beneath despair that borders on catatonic, we see signs of life, of a "dead but breathing" individual capable of animation.
But is this only confusing the picture?
A 2001 study cast doubt on the only feature of atypical depression that is mandatory under the DSM - that of mood reactivity. In their study, the authors evaluated the five symptoms of atypical depression across five different groups of patients (including women, different age groups, and according to severity and length of time of symptoms), and discovered mood reactivity only featured among the women patients, suggesting this particular criteria should be dropped.
The same study also found at best a limited association between the five atypical features among the five clinical profiles. Women, for instance, consistently displayed four of the five symptoms for atypical depression while patients under age 30 exhibited only one. Thus, we are left with the absurdity of two different sets of atypical patients exhibiting nearly mirror-opposite symptoms.
What is Going on Here?
Atypical depression represents a good faith attempt to separate out a significant group of individuals who are obviously experiencing depression, but not necessarily in the classic sense. In practice, psychiatry is retrofitting a set of diagnostic anomalies over the notorious DSM symptom check-list. Thus, before we can even determine if an individual has atypical depression, a clinician must first find evidence of "major depressive disorder." (Check-list depression, in other words.)
Then, in making a diagnosis of "major depressive disorder with atypical features" the clinician, in effect, is asked to contradict parts of that same check-list.
A 2010 abstract to a review article (the full article is in Japanese) tells us that we are probably looking at four views of atypical depression. The first two views attempt to separate out unipolar depression into a melancholic-atypical distinction. Thus:
- The Columbia University group (represented by the late Frederick Quitkin et al) sees mood reactivity as the decisive factor in atypical depression.
- The New South Wales University group (led by Gordon Parker) emphasizes anxiety symptoms over mood symptoms and the significance of sensitivity to interpersonal rejection.
The second two views interpret atypical depression as part of a unipolar-bipolar distinction. Thus:
- The Pittsburgh University group (which includes David Kupfer and Michael Thase) sees vegetative symptoms and lethargy as tip-offs to bipolar disorder.
- The soft spectrum group (led by Hagop Akiskal) would include some version of atypical depression in the bipolar spectrum (which regards some "unipolar" depressions as types of bipolar).
SIGN UP FOR MY FREE EMAIL NEWSLETTER
To give you an indication of the complexity of the discussion, following is a representative segment of one sentence of the abstract:
...reflects the theory that mood nonreactivity is the essential symptom of "endogenomorphic depression", which was proposed by Klein as typical depression.
The original Japanese would have been no less confusing, a point which the author seems to happily acknowledge. Indeed, the abstract resolves into brutal clarity in its summary dismissal of the diagnosis:
Consequently, the concept of atypical depression has become overextended and gradually lost its construct validity.
Basically, it's back to the drawing board:
The diagnostic criteria for atypical depression should be reconsidered in reference to various definitions and concepts and refined through accumulated clinical research.
Why This Conversation is Important
Since the introduction of first-generation antidepressants more than 50 years ago, clinicians and researchers observed that certain patients responded better to one class of medications than others. Thus, the title to this 1962 journal article:
The treatment of anxiety states and atypical depressions by the monoamine oxidase inhibitor drugs.
Monoamine oxidase inhibitors (MAOIs) such as Nardil give a boost to the dopamine system, as well as the serotonin and norepinephrine systems. By contrast, the other class of antidepressants of the era - tricyclics such as imimpramine - only acted on serotonin and norepinephrine.
A study by Quitkin et al published in 1993 in the British Journal of Psychiatry found a response rate of 72 percent for patients with atypical depression on the MAOI Nardil compared to 44 percent on imipramine.
I'm sure you see where this is going:
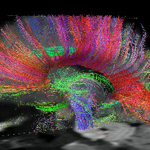
Any med that enhances dopamine firing acts as an energizer. In an optimum case scenario, increased dopamine signaling would restore pleasure, anticipation, and thinking in the limbic-cortical pathways of the brain. Thus, individuals experiencing vegetative symptoms in their depressions would come to life.
The catch is MAOIs have burdensome side effects compared to tricyclics and extremely burdensome side effects compared to the newer SSRIs such as Prozac and SNRIs such as Effexor. Thus, MAOIs are typically regarded as a treatment of last resort. But all bets are off if the depression is atypical.
A smart clinician is not limited to MAOIs. There are other meds for booting up the dopamine system, even if they are not indicated for depression. These would include meds indicated for Parkinson's, ADD, and narcolepsy.
The evidence base is slim for treating atypical depression with off-label dopamine-enhancers, and there are no guarantees. But the rather underwhelming response rates of antidepressants in general indicates the folly of prescribing an SSRI or SNRI for everything under the sun that resembles depression.
One important twist to this: If an atypical (or vegetative) depression points to a bipolar depression or a "unipolar" depression in the bipolar spectrum, then the first option may be a mood stabilizer rather than a dopamine enhancer. In treating bipolar depressions, clinicians and patients always need to be mindful of the next phase of the cycle. Being on an energizing agent when one is cycling up may not be a good idea, or - at the very least - is something to think about.Trying to Make Sense of This
Elsewhere on this site (including this article) I argue in favor of separating out depression according to vegetative features and agitated features. A typical-atypical distinction may well be more accurate, but hardly at the present moment, when even the experts cannot arrive at a working consensus.
In the current discussion over what constitutes atypical, psychiatry has lost sight of the fact of how the term came about in the first place - as a hypothesis for why certain patients with unipolar depression responded to MAOIs rather than tricyclics.
Let the conversation build on that important piece.
Reviewed June 17, 2016
NEW!
Follow me on the road. Check out my New Heart, New Start blog.