Populations
 POSTPARTUM DEPRESSION
POSTPARTUM DEPRESSION
Widespread ignorance gives this condition far more power than it deserves.
by John McManamy
Widespread ignorance gives this condition far more power than it deserves.
by John McManamy
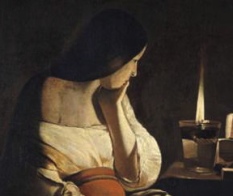
"A FEW WEEKS after I gave birth to my son," wrote Pamela Gerhardt in the Washington Post, "I rocked him gently to sleep, lay him in his crib, walked down the stairs, grabbed the vacuum cleaner and hurled it out onto the front lawn. It sat there all day, broken, the hose hanging from the blue spruce, the plastic pieces scattered on the lawn like tree limbs after a hurricane."
Welcome to postpartum depression, a condition that can ambush hopeful new mothers at the time when they least expect it and turn their dreams of parenthood into the worst of nightmares. The term postpartum merely refers to the triggering event. This is major depression, pure and simple, but with this cruel twist: A combination of ignorance and misplaced expectations - both on the part of the new mother and those who should know better - conspire to cause far more suffering than necessary.
"Bookstores file postpartum depression under psychology," Pamela Gerhardt notes in her article. "And how many women, giddy with the thought of becoming a mother, are perusing the mental illness section of Barnes & Noble?"
One guidebook offers this advice: "Treat yourself to a dinner out ... put on makeup." Another recommends a little mascara.
Weeks of mental anguish for Pamela followed, so she decided to consult a psychologist, who advised her to "shop at Nordstrom." Her obstetrician recommended she and her husband make more time for sex.
"A few weeks after demolishing that vacuum cleaner," she wrote, "my violent eruptions abated, only to be replaced by something far darker. I began to feel as though I was sinking, under the ground, not of this world, a feeling very similar to the one I'd had when my mother died ten years earlier."
What We Know About Postpartum Depression
Postpartum depression affects more than ten percent of mothers, with biology and environment contributing to its cause.
SIGN UP FOR MY FREE EMAIL NEWSLETTER
During weeks eight to 38 of pregnancy, progesterone levels increase seven-fold, estradiol 130-fold, and prolactin 19-fold, then drop sharply following delivery to pre-pregnancy levels. Also implicated are adrenal steroids, which affect cortisol which regulates the metabolism of food, and the thyroid.
Many women get better when their hormonal levels soon return to normal, but others can suffer for months or even years.
Women with a history of depression are at greater risk, as are those who react negatively to their weight gains and those with low self-esteem. Poverty and family upheavals also play a role, and studies have linked postpartum depression to traumatic birthing experiences, such as C-section or early hospital discharge.
In addition, the social isolation new mothers face in modern society has been fingered as a culprit.
Some form of mild depression strikes most new mothers. Up to 40 percent of new mothers actually experience indifference toward their babies within a day or so of delivery, though the duration is thankfully short, about three days.
Then there are the "baby blues," affecting some 50 to 70 percent of new moms, with onset occurring within three days to a month after delivery, and a duration of less than ten days.
At the other extreme is postpartum psychosis, affecting one in 500 births, accompanied by hallucinations, delusional thoughts, and agitated behavior. The mother cannot care for her baby, and there is serious risk of both suicide and infanticide. Women with bipolar disorder are at particular risk (with odds of one in five).
The Horror Stories
In August 2000, Suzanne Killinger-Johnson, 37, a Toronto medical doctor practicing as a psychologist and described by a fellow former medical student as a woman "every guy at med school had a crush on," jumped in front of a subway train with her six-month-old baby in her arms.
Ironically, her mother, also a psychotherapist, had written a book that contained this quote: "A lot of folks don't know what's cooking until the pot boils over."
Nearly a year later, Texas mom Andrea Yates, 36, got the attention of the entire US when she drowned her five children in the bath tub. Husband Russell said, "She loved those kids."
But not everyone was as sympathetic. NY Post columnist Andrea Peyser, for example, accused Andrea Yates of "methodically and diabolically" drowning her kids, going on to say many mothers kill their kids because they don't love them, and concluding with: "Still, blaming a mother for murder is heresy among the talking heads who fill the airwaves with psycho-babble about postpartum depression."
Andrea Peyser's portrayal of mothers as cold-blooded killers fails to account for those who simply commit suicide, leaving their bereaved families to pick up the pieces.
At about the same time of the Yates tragedy, Melanie Stokes, from the Chicago area, jumped to her death from a twelfth story hotel window several months after her baby was born. According to Melanie’s mother: "She stopped eating, she couldn't sleep, she was very agitated. She told me that she felt like a walking zombie. She told me she was a living corpse." According to an AP article, Melanie was hospitalized and diagnosed with postpartum psychosis, but later sent home.
The same AP article goes on to say that in the UK, all new mothers are evaluated for postpartum depression before they are sent home, and nurses make two mandatory home visits to check for symptoms within 40 days of childbirth. In the US, New York and New Jersey are the only states that require hospitals to give mothers information on postpartum depression.
Conclusion
Postpartum depression affects some 10 to 15 percent of deliveries. In the words of Pamela, in the Washington Post:
One day I was walking alone with my 10-month-old in the stroller, merrily pointing out the pretty leaves and the neighborhood doggies when I began to think about the devastating effect my suicide would have on my boy's life. I stopped in my tracks. This was the first concrete thought I had had of actually taking my own life. I made an appointment to see a psychologist – a new one – the next day.
Pamela finally got the help she needed, but much of her suffering simply did not have to happen.
Postpartum Depression Guidelines
If you are a mom-to-be or a new mom (or her SO):
- Treat postpartum depression as a potential part of the birthing and parenting process, and learn as much as you can.
- Have your doctor screen you for depression, whether you feel you need it or not.
- Don't overburden yourself. You don't have to keep up appearances.
- Get help from friends and family. Make friends with other parents.
- If you suffer from bipolar, prepare yourself for the possibility of postpartum psychosis, and have your support systems well in place.
- Postpartum depression responds to antidepressants, talking therapy, and group support. Do not be afraid to get help.
- If you are breastfeeding: Small amounts of SSRI antidepressants find their way into baby's milk, but not enough to be considered unsafe.
For further info, please check out Katherine Stone's excellent blog, Postpartum Progress.
Published 2000, reviewed Jan 4, 2011 and Dec 4, 2016
NEW!
Follow me on the road. Check out my New Heart, New Start blog.