Behavior
 NO PLEASURE, NO REWARD
NO PLEASURE, NO REWARD

No pleasure is a core feature of depression. Then what?
by John McManamy

No pleasure is a core feature of depression. Then what?
by John McManamy
READERS may recall Hall of Fame quarterback Terry Bradshaw’s public disclosure in 2003 of a decades-long depression. Out came the startling revelation that "I didn't understand that after every Super Bowl victory, I could never find pleasure in what I'd done."
Fame and fortune may not buy you happiness, but even an existentialist knows you're supposed to feel elated after leading your team to a Super Bowl victory. This lack of ability to experience pleasure or be interested in pleasurable activities (anhedonia) is as intrinsic to depression as feeling sad, so much so that without one or the other diagnostic citizenship is denied.
If you think of Terry's brain as a computer, his software was basically filtering out all that should have brought him any sense of accomplishment and joy.
I know the feeling. In late 1998, I was on a collision course with a suicidal depression. In previous years, around Christmas time, I had made gifts for my niece and nephews. One year it was watercolors of dinosaurs playing basketball (try to imagine a brontosaurus dribbling downcourt on a fast break). Another year I did an illustrated book. Yet another year I made papier mache masks, and the next it was a seven-foot tall cardboard and papier mache totem poll that you could take apart and reassemble. My piece de resistance was a miniature golf course with interchangeable putting surfaces for reconfiguring the holes.
I can't begin to describe the hours of pleasure those projects brought me, and how I much I looked forward to my once-a-year excursions from life as usual, where I would plot and scheme and plan and draw and buy new materials and go to the pantry where I had my art supplies stowed away in an old roasting pan. Then, out on the kitchen table, I could get down to the serious business of pretending I was Leonardo da Vinci.
But this year I couldn't be bothered. The pencils stayed in their drawers, the art supplies remained in the pantry. People Magazine's most glamorous woman could have called me saying she was lonely and I would have hung up the phone.
Anhedonia and Depression
Paul Keedwell MD of the Institute of Psychiatry (King’s College) goes so far as to define loss of pleasure as THE depression symptom. "I believe that the presence of anhedonia defines depression," he told this writer. "If one does not have anhedonia one is not depressed."
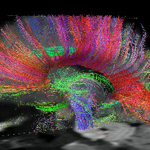
Dr Keedwell is the lead author of two complementary studies published in Biological Psychiatry in 2005. In an earlier article published in the Nov 2003 Advances in Psychiatric Treatment, Dr Keedwell and his co-authors point to a growing body of evidence that indicates that a breakdown in the brain’s reward system may play a key role in depression. From the mesolimbic region of the brain,dopamine-sensitive neurons project from the ventral tegmentum into the medial prefrontal cortex, amygdala, and ventral striatum. Reduced activity in the striatum may lead to a failure of the prefrontal cortex to process rewarding experiences.
As the authors explain: "The perception of reward would thus be reduced, leading to the core depressive symptom of anhedonia."
It can work the other way, as well. The medial prefrontal cortex may experience technical difficulties sending positive messages to the striatum.
To test this theory, Dr Keedwell and his colleagues recruited 24 individuals - half with major depression (all but one on meds), the rest healthy – and scanned their brains in an MRI while they performed tasks that included processing sad and happy lifetime memories.
A number of different brain regions reacted, but what caught the researchers’ attention was the ventromedial prefrontal cortex (VMPFC). DECREASED activity there was observed in healthy individuals in response to happy stimuli and INCREASED activity to sad stimuli. It was as if this part of the brain had to work harder to stay focused on sadness. In the depressed individuals this pattern was reversed; the VMPFC needed to go into overdrive to register any perception of happiness. Feeling sad, by contrast, just came natural. Something funny was going on.
SIGN UP FOR MY FREE EMAIL NEWSLETTER
The second study was an extension of the first, this time finding a similar correlation in happy (but not sad) responses in the VMPFC to various levels of severity of anhedonia (the Fawcett-Clarke Pleasure Scale measures for this). Again, the VMPFC had to work harder to process happy thoughts. Those with severe anhedonia also had weaker responses in the striatal regions. Clearly, the front and back ends of the brain were having trouble talking to each other. Whether the primary failure was in the VMPFC or whether the VMPFC was compensating for deficiencies in the striatal and other areas remains to be seen.
The authors placed great stress on the VMPFC and striatum being involved in the reward system of the brain. This raises the obvious question that maybe we should start throwing away our antidepressants and go with meds that crank up dopamine.
Dr Keedwell, however, cautioned this writer that meds that work solely on the dopamine system may be "too alerting" for some patients, while drugs such as amphetamines can be positively dangerous. Moreover, he pointed out that serotonin antidepressants may indirectly influence dopamine pathways. Further advances in imaging and pharmacogenomics may help us understand individual differences in antidepressant response.
Intriguingly, Dr Keedwell sees an overlap between anhedonia and apathy (see article), psychomotor retardation, and lack of drive. In the striatum, he informed this writer, there are many connections between the "limbic" and "motor" functions. The old functional distinctions in this region, based mainly on animal studies, may not apply to humans, he added.
Which raises the possibility of new distinctions, sharper diagnosis, and smarter treatments. Is your doctor aware of all this?
See also: Apathy.
Reviewed June 29, 2016
NEW!
Follow me on the road. Check out my New Heart, New Start blog.