Treatment
 ANTIDEPRESSANT TREATMENT STRATEGIES
ANTIDEPRESSANT TREATMENT STRATEGIES
Important considerations your doctor forgot to tell you.
by John McManamy
Important considerations your doctor forgot to tell you.
by John McManamy
THE BIGGEST FAULT with antidepressants lies in the people who prescribe them. Doctors (including psychiatrists) write scripts indiscriminately and send patients out the door with no equivalent of an operating manual, then go into denial when their patients complain.
A companion piece discusses five things you need to know. This article goes into greater detail on what your doctor should have told you. The following should not be interpreted as medical advice. I'm not in the business of dispensing medical advice, but then again, neither, apparently, are our doctors. Let's get started:
Antidepressant Side Effects
Onerous side effects are not a fair trade-off for an improvement in mood. Your doctor may tell you otherwise, but it is your throat the pills are going down, not his. You may have to put up with some initial side effects, most of which go away as your system adjusts. Since these effects kick in before the clinical benefit of the antidepressant you are almost certain to feel worse before you feel better.
Patience is advised, but so is vigilance. Keep your doctor in the loop.
Watch out for the ironic side effects, such as sexual dysfunction, weight gain, messed up sleep, or any effects having to do with quality of life, as these are likely to make your depression worse. It may be reasonable to accept six to twelve months of eunuch-hood, for instance, but you really need to see a substantial improvement in your condition to justify this. The thought of a life sentence with limited or no sexual function makes sense only to doctors, not patients or their loved ones.
As for sleep, mood and sleep are joined at the hip. Bad sleep is a reliable predictor of bad mood. Moreover, bad sleep is a symptom of depression. Over the long term, any side effect that worsens sleep is only going to worsen the depression.
The best decision a patient may make is going off his antidepressant. It may also be the worst one. There are no right or wrong decisions, only informed and uninformed ones
Antidepressants and the Bipolar Connection
Be mindful of persistent feelings of psychic unease or wanting to crawl out of your skin, even if your mood improves. Your doctor is likely to interpret an improvement in mood as a sign the antidepressant is working, and thus encourage you to continue the drug. Then, when the effects become intolerable, the doctor switches you to another antidepressant, then another. If anything, the depression worsens, with complications.
Years later, your doctor rediagnoses you with bipolar. By that time, it's impossible to tell whether you had bipolar all along or whether the antidepressant turned you - someone who had only experienced depression - into a walking basket case who now experiences bipolar symptoms. Only one thing is certain - you are now in much worse condition.
This unfortunate outcome is not uncommon. Speaking at a seminar at the 2008 American Psychiatric Association annual meeting, Frederick Goodwin, former head of the NIMH, stated that 50 percent of those with bipolar have been misdiagnosed by their psychiatrists, and that for one-third of those with a genetic disposition to bipolar "SSRIs have been terrible."
Another scenario is your antidepressant working too well too fast. This means you may be headed straight toward mania rather than normal. Despite the fact that the American Psychiatric Association's Treatment Guidelines stipulate that the bipolar diagnosis needs to be ruled out before issuing a depression diagnosis, too many clinicians are inclined to go with clinical depression as their default diagnosis.
Finally, beware of cycling in and out of depression. Your psychiatrist is likely to interpret the up phase of the cycle as your antidepressant working its magic, while absolving the drug of all blame as you crash back into depression. What is likely going on is that your antidepressant is speeding up your mood cycle, where you experience more ups, but also more downs. Technically, your ups may not qualify as bipolar, but you are cycling in a similar fashion, and your ups may eventually escalate. The best way to end the roller coaster ride is to slowly wean off the antidepressant.
Short Term
What you are looking for is any kind of noticeable boot-up to your brain, generally in about six weeks. The antidepressant may not deliver what you are looking for, but even a partial boot-up gives you something to work with. If enough neurons are firing, you may be motivated to get out of bed and embark on a healthy routine that encourages more neurons coming back online. (See the articles in the Recovery section.)
You need to be opportunistic about any boot-up. Relapse rates are notoriously high for patients on antidepressants, particularly for those who have only achieved partial recovery. You cannot afford to sit around and wait for your pill to do all the work, because the odds are overwhelmingly against you that it won't.
That initial partial boot-up may be all that you get from an antidepressant, and if that is all that happens you should regard the treatment as a success. Keep in mind that continued treatment may only make your condition worse, particularly if you represent bipolar waiting to happen. You may want to quit while you're ahead, but that is a matter you need to fully discuss with your (hopefully enlightened) doctor.
SIGN UP FOR MY FREE EMAIL NEWSLETTER
If Your First Antidepressant Doesn't Work
Clinical guidelines are based on the proposition that your first antidepressant has a good chance of failing. If that happens, the most authoritative findings we have (STAR*D) suggest that it is reasonable to replace the first antidepressant with a second one. Thus, the odds of at least partial clinical improvement go up from about 50 percent on one trial of an antidepressant to about 60 percent on two trials.
If Your Second Antidepressant Doesn't Work
The major surprise from the STAR*D trials was that two failures on antidepressants strongly predict the likelihood of a third failure. Third time may prove lucky, but you may have to accept the fact that you are likely to fall into that category of patients that psychiatry classifies as "treatment resistant." Rather than continuing to play endless rounds of pill roulette, it may be more prudent to revisit your diagnosis. This means paying close attention to the possibility of bipolar (or it's close cousin highly recurrent depression) or to personal temperament.
Medium Term
The best evidence we have indicates that quitting too soon on your antidepressant encourages relapse. The counter-argument to these kind of studies is that some of the returning depressions may be a rebound effect from quitting the antidepressant rather than a true relapse.
Long Term
The conventional wisdom that a person with depression needs to be on an antidepressant for life, analogous to a diabetic needing his or her insulin for life, is under serious challenge. A 2010 literature review by Giovanni Fava of the University of Bologna somewhat contradicts the findings of the 2003 Oxford study. Dr Fava argues that after six to nine months, antidepressants lose their ability to protect against future depressions and may make depression worse.
Over the long term, argues Fava, antidepressants may change the brain to the point of "oppositional tolerance," that may "propel the illness to a more malignant and treatment-unresponsive course." Reconciling the this finding with medium term findings indicates a six-month or longer period to buy time for antidepressants to work, for clinicians to tweak their treatments, and for patients to implement their own recovery routines. Beyond that, we're in No-Man's Land.
Dr Fava's oppositional tolerance hypothesis at present is a minority view begging further study. His hypothesis certainly offers a credible explanation for why those with recurrent and bipolar depressions fare so poorly over the long term, but, again, further study is needed (though you won't find any drug company funding a trial to discredit their product, which means Fava will be the best evidence to go on for some time to come.)
Likewise, long-term antidepressant efficacy is unproven. The evidence base is simply not there.
If you do relapse after going off your antidepressant, you are likely to get an "I told you response" from your doctor, with the not-so-implicit assumption of your irresponsibility. Yet, the equally common phenomenon of patients relapsing while on an antidepressant goes without clinical comment or embarrassment.
Antidepressant Treatment Strategies
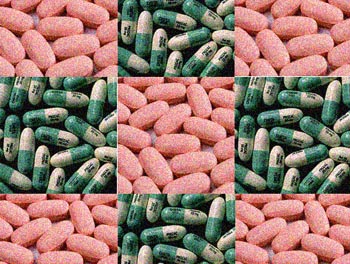
SSRIs (such as Prozac and Paxil, which target serotonin) and SNRIs (such as Effexor and Cymbalta, which in addition to serotonin also target norepinephrine), plus various antidepressants with novel actions such as Wellbutrin and Remeron, tend to be the meds of first choice. A smart clinician will attempt to distinguish between vegetative depressions and agitated depressions and dial in the prescription accordingly.
Wellbutrin, for instance, which has a modest dopamine action, is seen as an energizer. Remeron, which also doubles as a sleep med, is an obvious relaxer. The various SSRIs fall somewhere in the middle. The energizer/relaxer dichotomy also extends to augmentation strategies, such as boosting an antidepressant with an anti-anxietymed (such as Xanax), or a wakefulness agent (such as Provigil).
In cases of profoundly vegetative depressions (which may be a better and more accurate term than "atypical depression"), research clinicians have been known to reach back into the past for an MAO-I, originally viewed as an energizing med rather than an antidepressant. These meds, part of the early generation of antidepressants, have burdensome side effects, but have the advantage of targeting dopamine as well as serotonin and norepinephrine.
We do have meds that are robust dopamine agents. Unfortunately, they are expensive, illegal, addictive, and otherwise very bad for you. In lieu of a dopamine-specific antidepressant, clinicians have been experimenting with meds used for Parkinson's, ADD, and Alzheimer's, mainly as augmenters, or on as as-needed basis.
As for antipsychotics (which have the opposite effect of inhibiting dopamine but may indirectly boost serotonin), Eli Lilly led the field with a Prozac-Zyprexa combo (Symbyax) for bipolar depression. Later, Astra-Zeneca received an FDA indication for Seroquel to treat bipolar depresssion, followed by Bristol-Myers Squibb's indication for Abilify as an add-on treatment for bipolar depression. (Antipsychotics need to be used with extreme caution, but a persistent and severe depression that has not responded to standard treatment obviously justifies the risk.)
Undoubtedly, the best augmentation strategy is combining an antidepressant with cognitive (or similar) therapy. In one study, the response rates were an unheard of 85 percent.
There is a danger of "polypharmacy," but in the hands of a smart clinician the use of more than one antidepressant is justified. "California rocket fuel" - a combination of Effexor (or its successor Pristiq) and Remeron - offers a triple boost to the serotonin system, a double boost to the norephinephrine system, and a single boost to the dopamine system.
Meds Doses
Troublesome side effects may indicate that the dose is too high rather than something wrong with the med. Lowering your dose (under your doctor's direction) and monitoring your response is the advisable option. Some clinicians favor higher-than-recommended doses for maximum impact, though there is plenty of room for debate. What you really need to know is that we are all biologically unique and metabolize meds at different rates. SSRIs metabolize through the CYP2D6 enzyme pathway in the liver. This pathway may have more to say in how you react to your meds than what goes on with your neurons.
Weaning Off Your Antidepressant
Going cold turkey on your antidepressant incurs high risk of withdrawal symptoms (such as agitation and worsening of mood), especially with meds with a short half-life such as Paxil, and possible rebound depressions. A slow wean under a doctor's guidance is de rigeur, generally halving the dose over several days, then halving again and again. Paxil may require a more graduated wean.
An Irony
Over the years, I have favored the expansion of the bipolar diagnosis to embrace various forms of what we now describe as unipolar depression. Aside from a more accurate approximation of reality, a widened bipolar diagnosis would put clinicians on notice concerning their free-wheeling antidepressant prescription practices.
Critics of psychiatry have argued against the expanded bipolar diagnosis, which they perceive as a drug industry marketing tool. In reality, an expanded diagnosis would significantly reduce sales in one of Pharma's highest earners (antidepressants), which may explain why you won't see an expanded bipolar diagnosis in the near and distant future.
Thus, when it comes to antidepressants, we have antipsychiatry on the same side as the psychiatric and Pharma establishment. I can afford to laugh. Can you?
This is the final article in a five-part series on what you need to know about antidepressants. Previous Articles: Antidepressants - The Bad News First * Antidepressants - Right Med, Wrong Illness? *Antidepressants - The Chemical Imbalance Myth * Antidepressants - Five Things You Need to Know
Reviewed July 6, 2016
NEW!
Follow me on the road. Check out my New Heart, New Start blog.